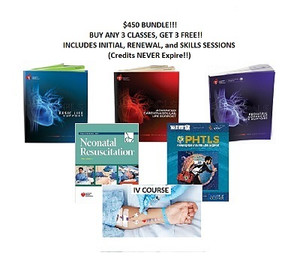
2025 - 6 CLASSES for $450 ACLS, BLS & PALS / AAP NRP, IV Certification, NAEMT PHTLS Bundle (INCLUDES Provider Manual E-Books!)
AHA, NAEMT, AAP, ARC, ASHI
NRP 2025 Guidelines Update
Umbilical cord milking
For most newborn infants who do not require immediate resuscitation clamping the umbilical cord should be deferred for at least 60 seconds 8th Ed 30-60 sec
2025 - Umbilical cord milking may be a reasonable alternative to deferred cord clamping in some scenarios where the newborn infant remains non-vigorous, the the umbilical cord is intact.
Greater than 35 Weeks - infants who remain non-vigorous despite 20 to 30 seconds of stimulation, milking the intact umbilical cord from the placenta toward the baby ( three to four times) may be a reasonable alternative to early cord clamping.
28 to 34 weeks - infants who remain non-vigorous, there is not enough evidence to recommend routinely milking the intact umbilical cord.
Less than 28 weeks - Intact umbilical cord milking is not recommended for preterm newborns infants because it has been associated with increased risk of severe intraventricular hemorrhage.
Procedure to milk the cord. compress the intact cord on the the placenta end toward the baby in a two to three second stroke that milks the blood in the cord toward the baby.
The cord is allowed to refill with blood and the procedure is repeated a total of four times.
FIO2 and Gestational Age Breakdown
>35 weeks Initial FIO2 / 21%
32-34 weeks FIO2 / 21% - 30%
<32 weeks FIO2 / 30% to 100%
Initial Peak Inflation Pressure
The suggested initial PIP is 25cm H2O
acceptable ranges for initiating ventilation on newborn are as follows
Gestational Age >32 weeks 25 to 30 cm H2O
<32 weeks 20 to 25 cm H2O
Rate of Ventilations
NRP 9th Edition says 30 to 60 breaths per minute
When to Begin Ventilation Corrective Steps
If the heart rate is not increasing within 15 to 30 seconds of starting ventilation and you do not observe chest movement, start the ventilation corrective steps (MR SOPA
This period has been extended from 15 seconds to within 15 to 30 seconds to allow proper time to assess.
Laryngeal Mask
A laryngeal mask may be used as a primary device for ventilation.
In most cases ventilation is initiated with a face mask or laryngeal mask.
In the 8th Edition the laryngeal mask was used as an alternative airway after ventilation is unsuccessful with a face mask or intubation.
Updated Target Oxygen Saturation Table
The Target Oxygen Saturation Table now starts at 2 minutes. Getting a reliable signal from the pulse oximeter can take 1 to 2 minutes from the time it's placed on the newborn's right hand.
2 min 65% - 70%
3 min 70% - 75%
4 min 75 % - 80%
5 min 80% - 85%
10 min 85% - 95%
Endotracheal Tube Size for Newborn Infants of Various Weights and Gestational Ages
<800 g 22-25 weeks 2.5 mm
800-1,200 g below 28 weeks 2.5 mm
1, 202-2,200 g greater than 34 weeks 3.5 mm
Point of Reference: Upper Gum
The new reference point is the upper gum. in the 8th edition is was the infant's lip.
Insert the endotracheal tube so that the marking on the tube corresponding to the estimated insertion depth is adjacent to the anterior edge of the infant's upper (maxillary) gum in the midline. This is updated to specify teh upper gum as the point of reference.
Endotracheal Tube Insertion Depth (Tip to Gum) for Orotracheal Intubation
Gestation Insertion Depth at Gum Baby's Weight
23-24 weeks 5.5cm 500-600 g
25-26 weeks 6.0 cm 700-800 g
27-29 weeks 6.5 cm 900-1000 g
30-32 weeks 7.0 cm 1,100-1,400 g
33-34 weeks 7.5 cm 1,500-1,800 g
The Neonatal Resuscitation Program® (NRP®) course conveys an evidence-based approach to care of the newborn at birth and facilitates effective team-based care for healthcare professionals who care for newborns at the time of delivery. NRP utilizes a blended learning approach, which includes online testing and hands-on case-based simulation/debriefing that focus on critical leadership, communication, and team-work skills.
The 9th Edition was released with the 2025 Guidelines.
The Neonatal Resuscitation Program (NRP) is an educational program of the American Academy of Pediatrics and is jointly sponsored with the American Heart Association (AHA). The course has been designed to teach hospital staff who care for newborns at the time of delivery, including physicians, nurses and respiratory therapists. Since the inception of the NRP in 1987, over 3 million individuals in the United States and a countless number of individuals abroad have been trained in NRP.
The NRP Provider Course introduces the concepts and basic skills of neonatal resuscitation. It is designed for health care professionals involved in any aspect of neonatal resuscitation, including physicians, nurses, advanced practice nurses, nurse midwives, licensed midwives, respiratory care practitioners, and other health care professionals who provide direct care during neonatal resuscitation.
Participants must complete the online test at www.aap.org/nrp and choose the 9th Edition ADVANCED NRP Provider Course for $75. Once the online Part 1 portion is complete, you will need to attend the in person hands on portion of the course. The cost of this course is $275 and includes the 9th Edition NRP E-Book.
CONTINUING EDUCATION
CE Accreditation and Credit Designation Statements:
Physician Provider
The American Academy of Pediatrics is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to
provide continuing medical education for physicians.
The AAP designates this enduring material for a maximum of 13.00 AMA PRA Category 1 Credit(s)™. Physicians should claim
only the credit commensurate with the extent of their participation in the activity.
This activity is acceptable for a maximum of 13.00 AAP credits. These credits can be applied toward the AAP CME/CPD Award
available to Fellows and Candidate Members of the American Academy of Pediatrics.
Physician Assistant Provider
PAs may claim a maximum of 13.00 Category 1 credits for completing this activity. NCCPA accepts AMA PRA Category 1
Credit™ from organizations accredited by ACCME or a recognized state medical society.
Nurse Practitioner Provider
This program is accredited for 13.00 NAPNAP CE contact hours of which 0.00 contain pharmacology (Rx) content, 0.00
related to psychopharmacology) 0.00 related to controlled substances), per the National Association of Pediatric Nurse
Practitioners (NAPNAP) Continuing Education Guidelines. The AAP is designated as Agency #A17. Upon completion of the
program, each participant desiring NAPNAP contact hours should send both pages of a completed certificate of attendance to ce@napnap.org. Payment of $15 for NAPNAP members and nonmembers is required via credit card for all NAPNAP
The Neonatal Resuscitation Program® (NRP®) course conveys an evidence-based approach to care of the newborn at birth and facilitates effective team-based care for healthcare professionals who care for newborns at the time of delivery. NRP utilizes a blended learning approach, which includes online testing, online case-based simulations, and hands-on case-based simulation/debriefing that focus on critical leadership, communication, and team-work skills.
Foundations of Neonatal Resuscitation
Key Points
- Most newborns make the transition to extrauterine life without
intervention.
- Before birth, pulmonary blood vessels in the fetal lungs are tightly
constricted, and the alveoli are filled with fluid, not air.
- Newborn resuscitation is usually needed because of respiratory
failure.
- The most important and effective step in neonatal resuscitation is
to ventilate the baby's lungs.
- Very few newborns will require chest compressions or medication.
- Teamwork, leadership, and communication are critical to
successful resuscitation of the newborn.
The Neonatal Resuscitation Program
The Neonatal Resuscitation Program (NRP®) will help you learn the
cognitive, technical, and teamwork skills that you need to resuscitate
and stabilize newborns. Most newborns make the transition to
extrauterine life without intervention. Within 30 seconds after
birth, approximately 85% of term newborns will begin breathing.
An additional 10% will begin breathing in response to drying and
stimulation. To successfully transition, approximately
• Five percent of term newborns will receive positive-pressure
ventilation (PPV).
• Two percent of term newborns will be intubated.
• One to 3 babies per 1,000 births will receive chest compressions or
emergency medications.
The likelihood of requiring these lifesaving interventions is higher
for babies with certain identified risk factors and those born before
full term. Even though the majority of newborns do not require
intervention, the large number of births each year means that timely
intervention can save many newborn lives. Because the need for
assistance cannot always be predicted, health care providers need to be
prepared to respond quickly and efficiently at every birth.
During your NRP course, you will learn how to evaluate a newborn,
make decisions about what actions to take, and practice the steps
involved in resuscitation. As you practice together in simulated cases, your team will gradually build proficiency and speed. The most gratifying aspect of providing skillful assistance to a compromised newborn is that your efforts are likely to be successful. The time that you devote to learning how to resuscitate newborns is time very well spent.
Why do newborns require a different approach to
resuscitation than adults?
Most often, adult cardiac arrest is a complication of coronary artery
disease. It is caused by a sudden arrhythmia that preve11ts the heart
from effectively circulating blood. As circulation to the brain decreases,
the adult victim loses consciousness and stops breathing. At the time
of arrest, the adult victim's blood oxygen and carbon dioxide ( C0 2)
content is usually normal and the lungs remain filled with air. During
adult resuscitation, chest compressions maintain circulation until
electrical defibrillation or medications restore the heart's function.
In contrast, most newborns requiring resuscitation have a healthy
heart. When a newborn requires resuscitation, it is usually because
respiratory failure interferes with oxygen and C0 2 exchange.
• Before birth, fetal respiratory function is performed by the placenta
instead of the fetal lungs. When the placenta is functioning
normally, it transfers oxygen from the mother to the fetus and
carries C0 2 away from the fetus to the mother. A healthy fetus
makes breathing movements, which are important for normal lung
growth.
• When placenta! respiration fails, the fetus receives an insufficient
supply of oxygen and C0 2 cannot be removed. Acid increases in
the fetal blood as cells attempt to function without oxygen and C0 2
accumulates.
• Fetal monitoring may show a decrease in activity, loss of heart rate
variability, and heart rate decelerations. If placenta! respiratory
failure persists, the fetus will make a series of reflexive gasps
followed by apnea and bradycardia.
• If the fetus is born in the early phase of respiratory failure, tactile
stimulation may be sufficient to initiate spontaneous breathing and
recovery. If the fetus is born in a later phase of respiratory failure,
stimulation alone will not be sufficient and the newborn will require
assisted ventilation to recover. The most severely affected newborns
may require chest compressions and epinephrine. At the time of
birth, you may not know if the baby is in an early or a late phase of
respiratory failure.
The content was explained well and I liked the knowledge checks to make sure I was understanding the information.
Na